It is 18 months since my application for ESA was approved and I was placed into the Support Group. Since that time I have been receiving ESA on time and have felt calm and reassured that the process was complete and that the DWP/ATOS had accepted my eligibility for the benefit on the basis of the evidence submitted by me and my doctors. I thought that all was in order.
Parkinson’s is a chronic, progressive and currently incurable disase. Chronic, because it is long-lasting. Progressive, because the disease process/symptoms worsen over time. Currently incurable, because despite advances in drugs or treatment (not all suitable for everyone with the disease, by the way), there is no cure, there is simply the potential to ameliorate some of the symptoms. Parkinson’s has a huge raft of symptoms, not everybody experiences all of them, but just Google and be shocked at the wideranging and individuality-killing nature of this disease. Parkinson’s is not (just) about tremor and publicly visible symptoms, but appears to set out to eradicate everything that made the individual who they were, how they appeared and what they were able to do. Once diagnosed and on the slippery slope of this disease, there is a constant battle, with the help of therapists and doctors, to maintain oneself as best as one can. Just look at all the pamphlets produced by Parkinson’s UK (linked here) and you’ll get an idea of just how all-intrusive this condition is.
Thus, coping with parkinson’s, like any other chronic, progressive and incurable neurological disease, is tough, but its a battle that those of us with it fight as best we can. In my case, currently, some symptoms are worsening, some seem to have plateaued for a while but a few new ones are making their presence known and requiring new medical management.
Someone living with such a disease in the UK is fortunate to have available a range of health and medical professionals, charities and support workers, to inform, encourage and help them cope with the disease process. As individuals with the disease, we have to try and be as positive and self-motivating as we can to deny the disease its hold over us. People with Parkinson’s, in particular, need a life that is calm, supportive, up-beat, positive and non-traumatic – it is in maintaining a positive equilibrium that they have every chance of being the best they can be in the circumstances. It doesn’t take much to disturb that equilibrium which results in an instant overload of coping mechanisms – beyond the control of the person with the disease and extremely shocking to them.
Stress, trauma, confrontation, hostility, noise and negative experiences all worsen the symptoms of those with parkinson’s.
People with parkinsonism, therefore do not need an unreasonable and inappropriate application and reassessment process for ESA, one of the key benefits available to them but, sadly, that is what happens at the moment because the French computer company, ATOS, is, in my view, signally failing to manage the DWP’s ESA benefits process in the fair manner expected of them by the public and Parliament. (NOTE: read earlier blog entries for background, starting here).
Once ESA has been granted to someone with a chronic, progressive and currently incurable disease and they have been put into the Support Group, that person is not going to stop needing to receive it…if anything, they are probably going to need more fiscal support and additional benefits. As far as State benefits are concerned, it is of course appropriate and reasonable that individual casefiles should be reviewed periodically, medical professionals should be invited to submit independent reports and, perhaps the individual themselves or their representative can be invited to review and confirm statements made in the past and that they remain valid and be given an opportunity to update the information held. A modification of the original application form for this purpose would be very straightforward.
That’s not what happens and this is how I know.
On 5 December 2013 a fat brown envelope from ATOS (on behalf of the DWP) arrived in the post.
Opening it and reading its contents instantly overstressed my system, sending me into windmilling tremor and tears. It was an 18-page form and its covering letter told me, as if for the first time, that my Incapacity Benefit was to be converted to ESA and that the form had to be completed for a full assessment of my eligibility for ESA – failure to complete the form will result in a suspension of benefits.
I couldn’t believe what I was reading – it was a duplicate of the paperwork received in 2012!! You’ve all heard and maybe seen the movie “Back to the Future” well… this felt like a weird form of time travel… and not in a good way.
All the stress of 2012 (NOTE: read my blogposts of that time) just flooded back. It felt as if the system had never granted me ESA and my being put in the Support Group had never happened. In one split second I am reduced to a physical and mental wreck and I can’t control the torrent of stress that tries to overwhelm me.
In case I am mistaken, I open my file of DWP paperwork and extract the letter and form I received in 2012 – fumbling and dropping the folder and pinching my fingers in the lever-arch clips as I do so – annd compare the new letter and form with those I received in 2012. The letter, apart from its date, is word-for-word identical and with a few minor changes the form is also the same.
I am immediately shocked and assume that somehow mmy original paperwork has gone missing – my system explodes with stress and tremor. I can’t think straight. Then… I think that perhaps the paperwork has been sent by mistake and I should have received a reassessment form instead. My mind is whirling at the threat of benefits being stopped and I wonder how I am to cope.
Once I have got my windmilling a little under control, enough to hold a telephone receiver, I call JobCentre Plus in Stratford. Still in mega stress (voice trembling, thoughts scrambling, hand tremoring) I explain the situation and am baldly told that I have to complete the form to apply for the benefit. I suspect I haven’t explained things clearly, given my stressed state, so I try again and say that I am already in receipt of ESA and was placed in the Support Group in 2012 so has there been a mistake in sending me an original application form again. I am then told, in a very matter of fact manner, that ATOS does not have a reassessment process, there is only one form of application for ESA assessment – the original one. The woman I am speaking with says that I will have to complete the initial application form all over again because, of course, failure to do so by the deadline of 3 January will result in suspension of benefits.
I am appalled – not only at the thought of having to try and complete such a big form as writing is now very difficult due to cramps and jerking – and ask why, if DWP/ATOS can’t create a reassessment form, doesn’t the cover letter at least make some reference to this being a reassessment. As it stands the paperwork is misleading and gives no indication that ATOS/DWP is aware that ESA has already been awarded. I am also a bit bewildered as it is as if the entire ESA assessment process is just beginning again, with all the worry and stress that involved (see previous posts).
A note of regret does seem to enter the voice of the person I am speaking with at this point, as she says that every day she and her colleagues are having to have similar conversations with many people with a wide range of progressive/incurable conditions but there is nothing any of them at DWP can do because it is ATOS that is tasked with administering the process.
I thank her for her time, replace the receiver and feel completely shell-shocked – what purpose can be served by just resetting the process in this way? Is ATOS simply making work for itself? I wonder what the process for a similar benefit would have been like in the past, when government administration was in public rather than private hands…not sure how to find this out.
Making a cup of coffee, rather sloppily as my system is taking ages to calm down, despite my best eforts, my initial terror/stress/tears segues into anger at a cruel and unfair system that is, once again, going to put me and probably my doctors through completely unnecessary hoops to prove once again that I am disabled with parkinson’s. Back on my bed (where I spend most of my time these days due to a range of gastric problems, due in part to parkinson’s) I feel nauseous, shaky, my labile blood pressure makes me feel unwell and my arms are jerking randomly but … I open Twitter and send this:

It is at least of some consolation that the Chairman of Parkinson’s UK agrees with me!
Time passes and the form is posted on 20 December, by Recorded Delivery, well in time for the stated deadline of 3 January 2014.
Completing the form took me more than a week – it is done in capital letters as I can’t write properly any more and I had to keep stopping as hand cramps kick in. It was tough. Tough not just because of the process of form-completion but because I had to revisit every aspect of my disability – seeing it written down was very fed-up making.
At every turn, after diagnosis, one is encouraged to try and come to terms with the changes brought about by symptoms. To accept, as best as one can, the inexorable erosion of ability in all things. To battle, with the help of medics, drugs and therapies, the worsening of symptoms. One is encouraged to look for what continues to be possible rather than to focus on what has become impossible. Having to reiterate the worst of one’s condition is like a little death – as the you that was is smothered by disease – and it makes one confront the reality that that things can’t ever be the same again. As one’s abilities deteriorate, actually completing the paperwork will become difficult, if not impossible… so what happens then?
Is this what a disability benefits process is meant to be? I am sure it wasn’t what the DWP intended when it appointed this private computer company to the task. Its certainly not what I expected of it.
Politicians on all sides forever speak of trying to create a fair society so surely, in a bid to create some kind of fair society for those whose diagnosed conditions are currently incapable of being reversed or cured and whose lives are already difficult enough, someone could devise a more practical ESA reassessment process? The current one is unwieldy and wastes a huge amount of effort, not just on the part of the disabled, but doctors and others called upon to contribute and, ultimately, on the part of those having to process unnecessary paperwork!).
It is very wrong, arguably bordering on cruel, to threaten such vulnerable people who are already in receipt of ESA with its cessation. There are many, like me, whose condition is directly worsened by the stress of this threat. There is something seriously wrong with a system that is trying to make everyone fit into a single “shape” simply because the computer company running the process, and being paid £80,000,000 (eighty million) a year for doing so, can’t be bothered to do the job properly. There has got to be a sensible way that the DWP and medical professionals can agree, once and for all, a straightforward and practical way of reassessing those individuals who have previously demonstrated beyond doubt their genuine entitlement to ESA/disability benefits and eligibility for the Support Group.
Each progressive/incurable condition has its own path to death, and each individual walks that path at a different pace, all the time trying to find ways to avoid the inevitable conclusion. In a civilised society there has to be a way of recognising that once on such a path of no return, the individual needs to be nurtured and supported by the entire system, including the benefits system – not threatened or browbeaten by it.
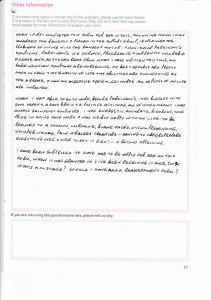
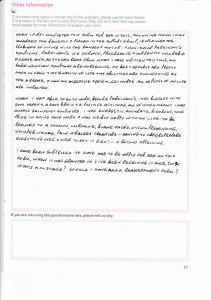
The ESA application form I received (remember, its not a reassessment form) ends with an Other Information section – this is how I completed it (I won’t tell you how long it took to write):
I have yet to receive any feedback or further information.
NOTE: the ESA award was continued until I was required to take early (medical) retirement in August 2014, at which point because I also got a small lump sum from my penson pot, my savings now exceed the minimum threshold for benefits. My monthly income is less than ever but I have to survive now until State Pension kicks in (if it still exists) when i am eligible for it!!
@joannekarma
#RCtheParrot